News Hub
The latest breaking stories
Access up-to-date news and information on a wide range of press releases including business, finance, technology, healthcare, entertainment, and more.
Discover the most important & comprehensive stories delivered directly to you daily.


- Business Finance
- 27/01/2026
- 20:26
With the Acquisition of Kaiser Associates, Sia Launches a Global Business Line Dedicated to Corporate Strategy, PE & M&A
NEW YORK–BUSINESS WIRE– Sia continues its US expansion with the acquisition of Kaiser Associates, a premier strategy consulting firm headquartered in the United States…
- Contains:


- Disability, Medical Health Aged Care
- 27/01/2026
- 19:42
Physical Disability Australia to host 4th annual Physical Disability Awareness Day – Sunday 1st February 2026
On Sunday February 1st 2026, Physical Disability Australia (PDA) will be hosting the fourth Physical Disability Awareness Day and you’re invited to join the…
- Contains:


- Medical Health Aged Care, National News Current Affairs
- 27/01/2026
- 18:27
University’s first medical students welcomed by Prime Minister
AustralianPrime Minister Anthony Albanesewas inDarwinto meetsome ofCharles Darwin University’s(CDU)School of Medicinefirststudents,reiterating the importance of theprogramto the Northern Territory insecuring thefuture health workforce. From February…
- Contains:


- Disability
- 27/01/2026
- 17:51
Making Australia’s Hate Speech and Vilification Laws Work for People with Disability
Disability Representative Organisations acknowledge the passage of theCombatting Antisemitism, Hate and Extremism (Criminal and Migration Laws) Bill 2026 (Cth)and the additional protections it introduces…
- Contains:


- Technology Innovation
- 27/01/2026
- 17:41
Artajasa, the Largest Operator of Indonesia’s QRIS, and Ant International Launch Global Payments and Digital Finance Partnership
SINGAPORE–BUSINESS WIRE– PT Artajasa Pembayaran Elektronis (“Artajasa”), Indonesia’s leading payment system infrastructure provider, has entered into a Memorandum of Understanding (MoU) with Ant International,…
- Contains:


- Sport Recreation
- 27/01/2026
- 17:12
Ohana Development and Manchester City F.C. Sign Agreement to Launch Multi-Billion-Dirham Project in Abu Dhabi
The 1.67 million square metre development is the world’s first Manchester City branded residential destination ABU DHABI, United Arab Emirates–BUSINESS WIRE– Ohana Development, a…
- Contains:


- Business Finance
- 27/01/2026
- 17:11
Cirium Ascend Consultancy Named Appraiser of the Year at the Aviation 100 Awards for a Record 11th Time
The fourth consecutive win recognizes Cirium’s position as the industry’s foremost provider of accurate, transparent aircraft valuations to the aviation finance and leasing sector.…
- Contains:
- Technology Innovation
- 27/01/2026
- 17:11
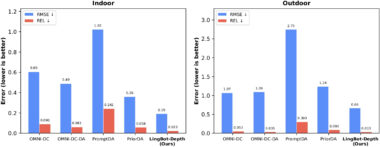
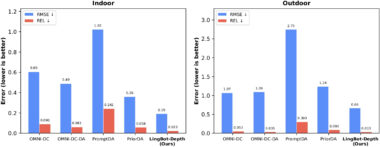
Ant Group Subsidiary Robbyant Unveils Spatial Perception AI Model LingBot-Depth
SHANGHAI–BUSINESS WIRE– Robbyant, an embodied AI company within Ant Group, today open-sourced LingBot-Depth, a high-precision spatial perception model designed to enhance robots’ depth sensing…
- Contains:
- Entertainment, International News
- 27/01/2026
- 17:00
Universal Studios Japan to Deliver Immersive Pokemon Experiences for Fans
OSAKA, Japan, Jan. 27, 2026 /Kyodo JBN/ -- On January 27, Universal Studios Japan, operated byUSJ LLC, and The Pokemon Company announced their plan to offer more innovative, immersive, and world-class Pokemon experiences. The project is part of Universal Studios Japan's ongoing effort to enhance its offerings and bring fan-first, trip-driving characters to the park. Image: https://cdn.kyodonewsprwire.jp/prwfile/release/M108172/202601212812/_prw_PI3fl_SEE5eL7J.jpg Universal Studios Japan is proud to build on its prior success and bring to life the world of Pokemon in new and enriching ways for the first time. Following its debut in Japan, Universal Destinations & Experiences will deliver unique Pokemon experiences across…
Media Outreach made fast, easy, simple.
Feature your press release on Medianet's News Hub every time you distribute with Medianet. Pay per release or save with a subscription.

